Artificial Pancreas
There are more than 4 million people in the UK living with diabetes. Someone is diagnosed with Type 1 or 2 diabetes every 2 minutes in this country, amounting to nearly 800 people every day. The disease brings an increased risk of going blind, kidney failure or heart disease.

For diabetics a sugary meal is potentially lethal because their bodies cannot correctly process the sugar in the food. Too much or too little sugar in the bloodstream can, in extreme cases, lead to a life-threatening diabetic coma.
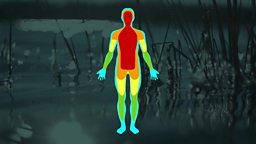
In a healthy person, the pancreas monitors the level of glucose in the blood and releases just the right amount of the hormone insulin. Insulin acts like a key that allows the glucose to enter the body’s cells, to be used for energy or stored for later.
In diabetics, this system doesn’t function properly. Many have to monitor their blood sugar level regularly, and inject insulin several times a day. One mistake or missed reading can have serious consequences.
But an innovative medical trial is under way that may transform life for many diabetics. For the first time, researchers have developed an artificial pancreas that can respond accurately to blood sugar levels and even predict the body’s insulin requirements.
The system consists chiefly of pre-existing off-the shelf components: a blood glucose sensor and an insulin pump, which is controlled remotely by a mobile phone. The breakthrough has been to get them working together to monitor glucose levels closely, and respond with an accurate dose of insulin with the help of a specially-designed phone app.
A team from the University of Cambridge led by Dr Roman Hovorka have been developing this new-generation artificial pancreas. The key difference between the new artificial pancreas and prior versions, is that it tries to mimic what the body’s pancreas does behind the scenes, reacting to the glucose level and changing the insulin delivery every ten minutes.
Perhaps the most ground-breaking innovation is an algorithm that predicts when insulin will be needed after eating. It works by building a record of how much insulin the patient needs after meals, and as the system gathers more information about that individual, it learns and adapts.
Hovorka believes that the potential benefits of the artificial pancreas to manage both Type 1 and Type 2 diabetes are huge. Diabetes consumes 10% of the NHS budget, mainly through the complications associated with the condition. Through improved glucose control, these complications and their impact can be reduced, and life expectancy increased.
This intelligent technology, which effectively learns from experience, is paving the way for a future in which artificial intelligence will transform medical practice.