Can organs be purpose-grown using stem cells?
Our vital organs can be damaged by accidents, disease, or simply wearing out as we grow older. For many, a transplant is the only option — yet transplants from donors carry a whole host of problems. There is always a lack of viable donor organs (in some countries there is no transplant programme at all), and even after a successful transplant the recipient needs to take drugs to prevent their immune system from rejecting it.
Many people think that the solution would be to repair our organs from inside our bodies - or to ‘grow’ entirely new organs from our own cells – a new field of science called ‘regenerative medicine’.
The key to regenerative medicine is the discovery of so-called ‘stem cells’
These are cells with the potential to develop into any type of cell - from a heart, to a lung to a skin cell. This potential means that they can theoretically be used to grow new tissues and organs.
Professor Macchiarini and his team have been working in this field for many years, and have been developing a means of replacing the trachea – or windpipe. The team are carrying out a clinical trial of a method which uses an artificial ‘scaffold’, made of artificial nanofibres and designed to mimic the natural shape and mechanical properties of a human windpipe as closely as possible, seeded with the patient’s own stem cells.
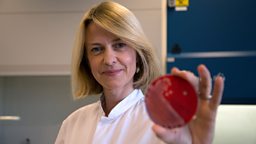
The first stage of the treatment is to extract bone marrow
This is a fairly routine medical procedure performed under general anaesthetic. ‘Mononuclear’ cells (cells with one nucleus) are extracted from the bone marrow and within these there will be some stem cells. Once the cells have been processed they are carefully dripped onto the scaffold. CT scans of the patient’s natural windpipe help the team ensure that the scaffold is as close a match as possible for size.
Once the scaffold is completely coated with cells it is put into a specially designed ‘bioreactor’ along with growth medium to encourage the cells to multiply. For two days, the team continuously monitor the scaffold to ensure it continues to rotate, carrying oxygen and fresh growth medium to the vital cells.
After 48 hours in the bioreactor, the cells on the scaffold are sampled to ensure that they are living and multiplying. If there are enough metabolically active cells the transplant can go ahead.
The damaged windpipe is carefully removed and replaced with the new scaffold, and once it is inside the body, the rest of the healing process takes place. Over the coming weeks, the cell-coated scaffold develops into a fully functioning windpipe. The theory is that when the cells on the scaffold die they send out signals which recruit new cells to the site, and these relatively quickly help form all the different cell layers that are needed to make such a relatively complex organ.
The technique
Development
The first trachea transplant using the patient’s own stem cells took place in Barcelona, in June 2008. It was carried out by an international team which included Prof Paolo Macchiarini and researchers from Bristol and Barcelona Universities, and the patient is still doing well. The first transplants used a donor trachea stripped of its own cells and coated in the patient’s stem cells rather than an artificial scaffold. Since 2011, Prof Macchiarini has been using synthetic scaffolds rather than donor windpipes.
Criticism
The procedure is not without its critics. Before any procedure is allowed in humans it’s necessary to carry out extensive trials in the laboratory, to ensure the new procedure is safe and effective. When the first stem cell trachea transplant was performed in 2008, several scientists voiced concerns that not enough pre-clinical work had been done to allow the transplant to go ahead. However, the surgery was approved by regulators in the U.K. and in Spain. Since then, Prof Macchiarini has received grants from the European Union and Russia to continue trialling the technique and has received U.S. Food and Drug Administration (FDA) approval to conduct the first such transplant in the United States.
There is debate within the scientific community about what happens to the stem cell coated trachea once inside the body. Critics of the procedure claim that there is no way of knowing whether the cells have developed into functioning wind pipe cells: see . Prof Macchiarini admits that they don’t fully understand the exact mechanism of how the trachea develops, but claims they do have evidence that healthy tissue grows on the trachea. . He is carrying out laboratory experiments to prove the technique works and to understand exactly what is happening at a cellular level. He plans to publish his conclusions together with the results of the trial.
There has been a lot of controversy about the mortality rates following the transplants, and allegations of professional misconduct have been made against Prof Macchiarini. These are currently the subject of investigation.